
On Halloween last year I was crippled with spasms in my back. Not the kind of spams that constantly hurt but the kind of spasms that literally, well . . . spasm! They come in waves triggered by any little barely perceptible movement.
My 17 year old son drove me to the doctor, helped me into the office and helped me pick up my meds all while panicking inside because he had never seen his mother immobilized by pain.
I couldn’t move! Couldn’t breathe! Couldn’t believe . . . It was my hip flexor!
There are two muscles that blend together to form your hip flexor muscles. The iliacus (il-ē-AK-us) and the psoas (SŌ-az). Together they are referred to as the iliopsoas (il-ē-ō-SŌ-az).

- The iliacus runs from your pelvis to your femur.
- The psoas runs from your spine ~ vertebra and discs ~ to your femur. It is the only muscle that connects your legs to your spine!
For more detailed info check out this video!
They are primarily responsible for lifting your knee up toward your chest or your foot off the ground. BUT they also play a role in stabilizing or moving your spine and pelvis in various situations . . . for example:
- The psoas helps to stabilize your spine

Iliacus Stabiliing - when you are sitting especially without back support
- or when you are carrying or holding something on the opposite side of your body
- The psoas can move your spine ~ either bending to the side or curling up
- The iliacus helps to stabilize the pelvis when you are standing on that leg and the other leg is extending behind you.
- They both work when you are performing a sit up (and you thought that was working your abs didn’t you!).
Whenever I see someone with back pain, I always look at the hip flexors to make sure they are as they should be ~ strong, flexible and being used appropriately. Nine times out of 10 they are not, regardless of the origin of the back pain. And at least 50% of the time they contribute to or are the source of the back pain! Why?
Well lets first consider the origin of these muscles ~ they attach to the vertebra and the discs in the spine, they are very deep muscles not near the surface of your hip or abdomen ~ so it is logical from an anatomical perspective that this would cause the back to hurt.
The way that the core muscles attach creates a system of stability around the spine and pelvis assuming that everything is as flexible and strong as it should be . . . for reference your core muscles include the abdominals, the gluteals, the hip flexors, back extensors, and if we are getting detailed all the muscles that function at the hip and spine.

If your abdominals and glutes aren’t helping to stabilize your back when you lift, bend and twist then the hip flexors have to help too much and are overused. This pulls your lumbar spine forward (Lumbar Lordosis) and impacts alignment.
If your hip flexors or back extensors are too short or tight they can pull your spine forward increasing the arch in your back and compressing your joints and disc. Again this pulls the spine forward (Lumbar Lordosis) changing alignment. 
So how do you injury your hip flexors?
- Athletes or active folks usually do something traumatic like straining them while kicking a ball, they over use them when walking up a hill or lifting incorrectly.
- Sedentary people may overuse them when sitting too long, standing or sitting with improper posture or lifting incorrectly.
- Finally some people are just built in a way or have developed movement habits that tax or activate hip flexors preferentially over other more appropriate muscles and then eventually . . . ouch! (This is me :D)
Now that you know the different components affecting the hip flexor, you see that there may be a few different sites or locations of pain, but let’s talk about one specific source ~ the muscle itself. When you injure or overuse a muscle it develops these little pesky muscle knots called trigger points . . . these guys send all kinds of signals all kinds of places and make you think the pain is located in one place (Your Back) when it’s actually coming from another (Your Iliopsoas!). This is referred pain: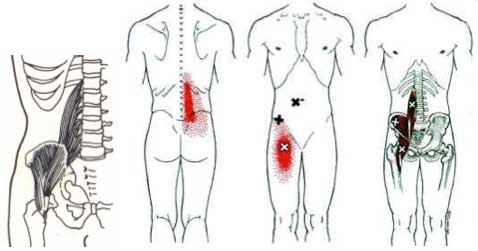
Why does one person feel it in the back and another in the front ~ its based on how we are wired.
If you have postural imbalance, weakness or tightness, and overdo a sport/activity or stay still too long, you create movement dysfunction which only feeds the beast!
So . . . are you surprised, confused, feeling pretty smart because you already knew this?
If you have this type of problem I will be discussing how to deal with it so stay tuned . . .
If you know someone with back pain share this post.
I invite you to comment below . . . and email, text or call with questions!
424.247.6987
Be well! Roxi
 Hopefully you are feeling like you made a great choice ~ I don’t suspect you are necessarily happy with needing surgery and the coming rehabilitation but now that your joint is stable again proper healing can begin ~ its uphill from here baby!
Hopefully you are feeling like you made a great choice ~ I don’t suspect you are necessarily happy with needing surgery and the coming rehabilitation but now that your joint is stable again proper healing can begin ~ its uphill from here baby!







 I know the rest of the week holds hiking and water activities, shopping and more. Of course there is the long drive home as well (sigh). So what will happen when I get home?
I know the rest of the week holds hiking and water activities, shopping and more. Of course there is the long drive home as well (sigh). So what will happen when I get home?
